Q&A with Cam
Learn what might be behind your symptoms
Who are the people most likely to present with Anterior knee pain?
One of the most common issues with the front of the knee is patellofemoral joint (PFJ) pain.
PFJ pain is typically caused by poor alignment and control between the lateral and medial quadriceps, as well as the hip-to-knee angle (Q angle), which can be influenced by genetics or growth patterns during adolescence. .
This condition presents as sharp pain behind the kneecap, a sandpaper-like sensation, increased pain when walking downstairs, difficulty squatting, and discomfort during prolonged sitting with knees bent..
PFJ pain is more common in adolescent girls due to a wider Q angle.
Additionally, Osgood-Schlatter syndrome, affecting adolescents during growth spurts, involves pain and strain at the tibial tuberosity where the patellar tendon attaches.
Treatment typically involves activity modification, stretching, and pain relief, and the condition usually resolves on its own.
How do you help people manage anterior knee pain?
When experiencing anterior knee pain, the best course of action includes:
- Ease pain in your knee with application of Ice
- Add compression when swollen, or for additional support
- Release your ITB/Lateral Quadriceps
- strengthening the Vastus Medialis Oblique muscles (VMO)
- improving hip abduction strength and lumbopelvic stability
- addressing any hip mobility restrictions.
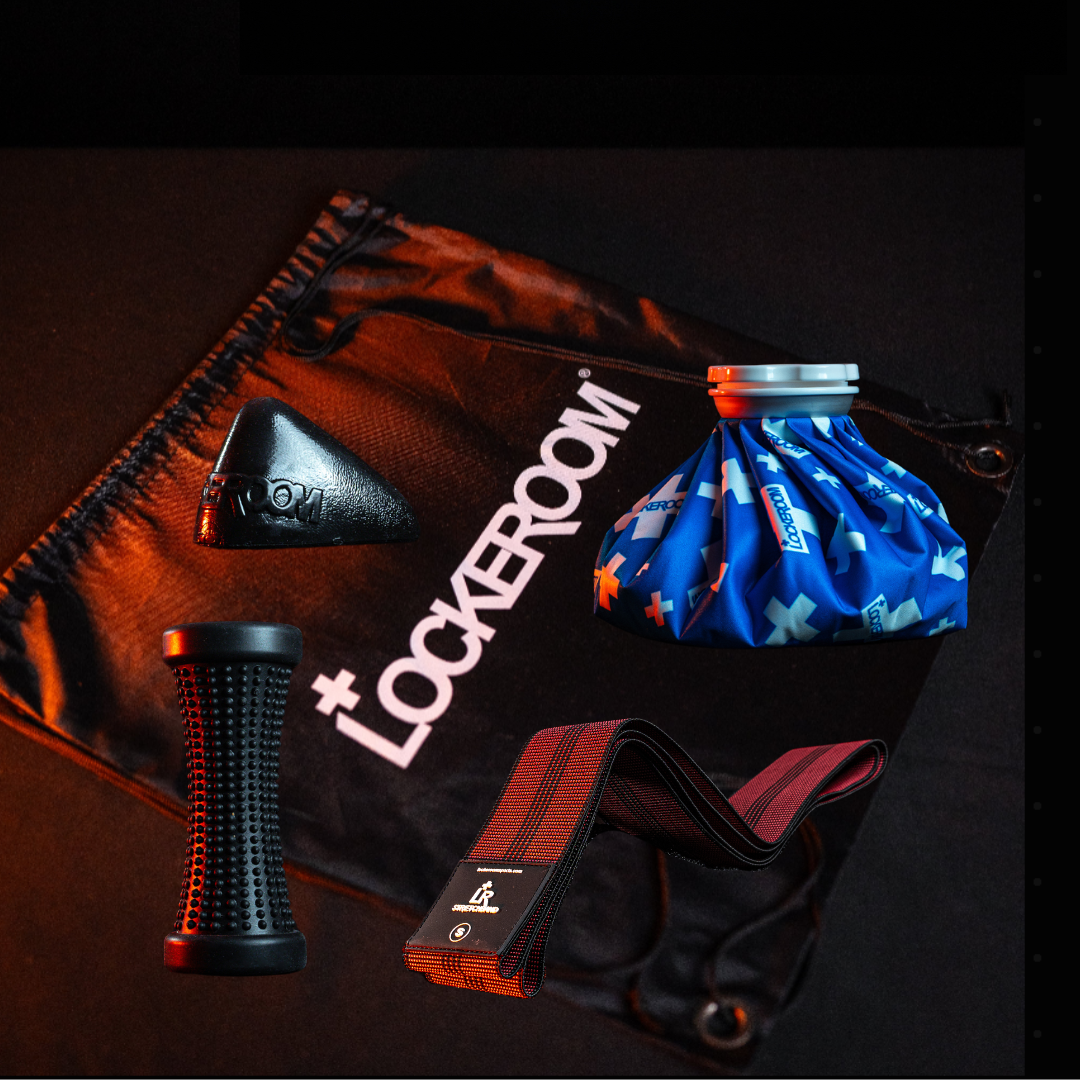
Begin by using a Foam roller or Footeez roller to reduce ITB tightness, release muscle tightness in the TFL and Glutes with a Pocket Physio Max trigger, and stretch your Quads and ITB with a Stretchband.
Additionally, applying ice and compression with an Ice Mate can help manage pain and support recovery.
What kind of trauma injuries occur in the anterior knee?
Traumatic injuries to the anterior knee include patella dislocations and less frequently, patella fractures. Patella tendon and quadriceps tendon ruptures are not uncommon.
A patella dislocation occurs when rotational forces cause the patella to move out of its normal position on the lateral side of the knee, often spontaneously reducing on its own. However, if the patella does not return to its proper position, gentle knee extension may be required. This can be very painful. This injury can happen to anyone, often involving a forceful twisting action, such as during running and changing direction.
A patella fracture typically results from a direct fall onto the front of the knee on a hard surface. Depending on whether the fracture is displaced or non-displaced, treatment may range from conservative management to surgery. It is essential to be assessed by a surgeon to determine the best course of action.
Tendon ruptures are often surprising events ie no prior problems reported.
For all these traumatic injuries, the best course of action includes immobilizing the knee, applying ice with an Icemate to manage pain, and seeking immediate medical evaluation.
Fractures and tendon ruptures should be referred directly to an orthopedic specialist, while dislocations can be evaluated by a doctor or allied health professional. Typical treatment of a knee dislocation involves an external brace for a period of 4-6 weeks with strengthening exercises and patella taping.
How long before I can play again if I have dislocated my kneecap?
A typical return to activity timeline following a patella dislocation is 6 to 12 weeks post-injury.
The recovery time for a patella fracture, whether managed operatively or non-operatively, typically ranges from 6 to 12 months before returning to play.
The return can be challenging due to the nature of the injury. Tendon injuries can take a similar time as for fracture recovery.