News
What does a diagnosis really mean?
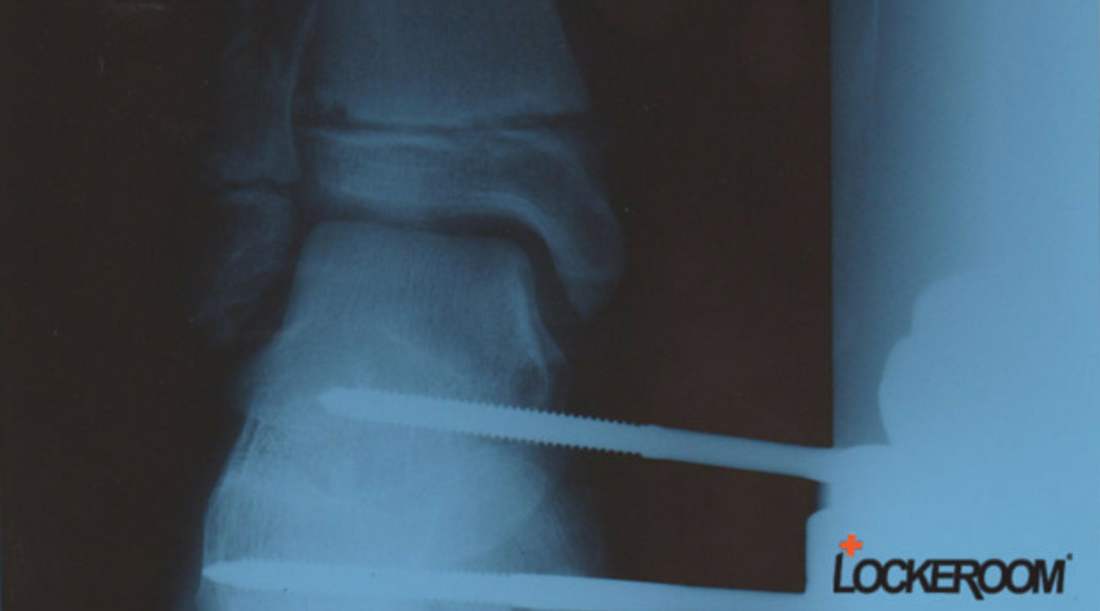
This diagnostic image clearly shows a fracture. As a Physiotherapist, this type of information is presented to me by patients, daily.
What the image doesn't tell is that it was a medial compound fracture of the tibial growth plate of a 14 year old boy caused when he fell from a flying fox (although the screws of the external fixator should be a give away!)
Yet I know all about this injury.
I know what action preceded the moment of impact, what forces were in play at the time of injury, the other injuries this person suffered, their state of mind at the time, and their ongoing fear of re-injury throughout their recovery journey.
I know, because this is an X-ray of my son's leg and I was there when he broke it.
But what if I wasn't and this was the only diagnostic tool given to me by a patient?
To create an effective rehabilitation plan and set realistic recovery milestones, I need to know the rest of their story, the part that is not written on a diagnostic report.
Not the circumstances of how they hurt themselves, that's easy to find out. I need to know what other physical forces were in play that may have contributed to their injury or will continue to impact their recovery.
It is imperative for treating therapists to return people to a level of function that minimises their risk of re-injury.
To get a patient back to 'normal' function following injury, you need to establish what their 'normal' was prior to injury. And if their 'normal' function places them at risk of re-injury, you need to develop a plan to improve their dynamic movement patterns, to reduce this risk.
Both you and your patient must clearly understand the consequence of the diagnosis. In other words, if the diagnosis is the starting point that brings you and your patient together, your treatment plan must be a mutually agreed 'what now'.
Don't just treat locally and manage pain. Managing globally, to eventually improve dynamic movement, is an integral part of recovery.
Of course, the primary injury should be of upmost consideration when addressing any biomechanical issues that may have contributed to or will effect recovery. This is certainly not a new concept but in my experience, it's just not always considered as an essential component of a treatment plan!
If a patient presents with patello-femoral pain for example, you can't just treat anterior knee pain. To be effective you must assess and correct lower limb biomechanics.
In a clinical environment upright postures are often assessed in a stationary stance position but they must be looked at in dynamic movement as well, because that's where you are going to see the forces at play.
Rehab progressions must be based around what you observe.
Developing a keen eye for 'normal' patterns of movement allows more accurate identification of abnormal patterns, in both simple muscle activation and control in dynamic movement.
Ensure that restoring a patient's elastic energy is a key priority of your treatment plan and that the milestone is met, before allowing them back to play sport!
Usually the starting point of treatment is reducing patient discomfort but at the same time you should consider addressing any other functional deficiencies identified.
If a scan reports an area of Trochlea damage from lunging in a particular sport, clearly you have to address the direct problem i.e. the lunge lesion but you also have to address any other contributing factors that may have increased their vulnerability to this type of injury.
Always look in either direction from the injury to identify deficiencies in mechanics, stability and proprioception. If the injury relates to the knee, look at the ankle and the hip and pelvic function in dynamic movement. The clues will be there!
If you are observing a patient perform a 'normal' dynamic movement pattern such as walking, and they exhibit 'abnormal' function i.e. foot pronation or poor hip control, dig into their history a little. Ask questions!
Their history is most often likely to tell you that they've had many previous issues ie MTSS, muscular injury to lower limb ie calf strains or hamstring strains. This is the untold story of their diagnosis, and the key to your treatment plan.
To achieve effective outcomes and strengthen your professional reputation, always treat the patient, not just the injury!

















 Designed in Australia
Designed in Australia